-
Changing the Pattern: Asthma Inhaler Use, Societal Costs, and Health Benefits
Certain asthma inhalers have a significant carbon footprint. But substituting with a different inhaler type could both decrease harmful emissions and be cost effective.
The Problem
Inhalers are a key mechanism for the treatment and control of asthma, which affects hundreds of millions of people worldwide. Somewhat surprisingly, they can also be a source of greenhouse gas (GHG) emissions.
One of the most commonly used inhalers, the metered-dose inhaler (MDI), uses propellants known as hydrofluoroalkanes (HFAs) to deliver medication to a patient’s lungs. HFAs are potent GHGs, and while the emission amount of a single MDI use may be small compared to other emission sources such as vehicles or power plants, HFAs can contribute significantly to climate change: They carry a global warming potential that is 1,300–3,350 times that of carbon dioxide.
Because of the combination of global population growth and the increased prevalence of asthma, demand for MDIs is projected to increase, and so too will their impact on the environment.
A Solution?
Fortunately, another commonly used inhaler – the dry powder inhaler (DPI) – does not use HFAs and has a much lower carbon footprint. This raises two important questions:
- How much could substituting DPIs for MDIs help reduce inhalers’ overall climate footprint?
- What are the cost-benefit trade-offs of such a substitution for governments and society at large?
To date, studies of the GHG emissions of different asthma inhalers have been conducted only for individual countries. The global nature of climate change, however, calls for a similarly global estimate of the impact of inhalers on the environment.
To fill that gap, a team from Analysis Group partnered with researchers from Novartis to quantify the global impacts that substituting DPIs for MDIs would have on GHG emissions, health, and costs.
Accounting for Carbon, Cutting Emissions
Determining whether substitution of DPIs for MDIs is cost effective requires more than a simple comparison of the prices of the two devices. To account for the damage done by GHG emissions, we also incorporated two US government estimates for the social cost of carbon* (SCC):
- A baseline SCC
- A high-impact SCC, representing higher-than-expected economic impacts from climate change
We added the cumulative SCC estimates to our calculations of substitution costs based on three scenarios for inhaler use over 50-year and 10-year time horizons:
Scenario A
Status quo – no change in current patterns of inhaler useScenario B
DPI market share increases by 2% per yearScenario C
DPI market share increases by 5% per year
In both Scenario B and Scenario C, emissions were significantly lowered by switching from MPIs to DPIs, regardless of whether we looked at the short-term (10-year) or long-term (50-year) horizon.Assessing the Economics of Inhaler Use
Turning to the cost side of the equation, we found that in both scenarios, replacing MDIs with DPIs resulted in higher costs for inhaler use, with higher-cost DPIs making up more of the usage costs.
The picture changed, however, when we added SCC estimates to inhaler costs to come up with total societal costs for both scenarios. We found that, using the high-impact SCC over the 50-year timeline, the GHG emissions and total SCC impacts of inhalers declined under both substitution Scenarios B and C (relative to the Scenario A status quo), resulting in lower total costs for each substitution scenario compared to the status quo.
Emission costs were also reduced, although not as much, over the 10-year horizon using the high-impact SCC estimates and over both time periods when using the baseline SCC estimates. In these scenarios, the increased costs for inhaler use led to modestly higher total costs when compared to the baseline scenario. In the aggregate, we can conclude that the long-term reduction in environmental damage mitigates, to an important extent, the drug costs associated with inhaler substitution.
Improving Health
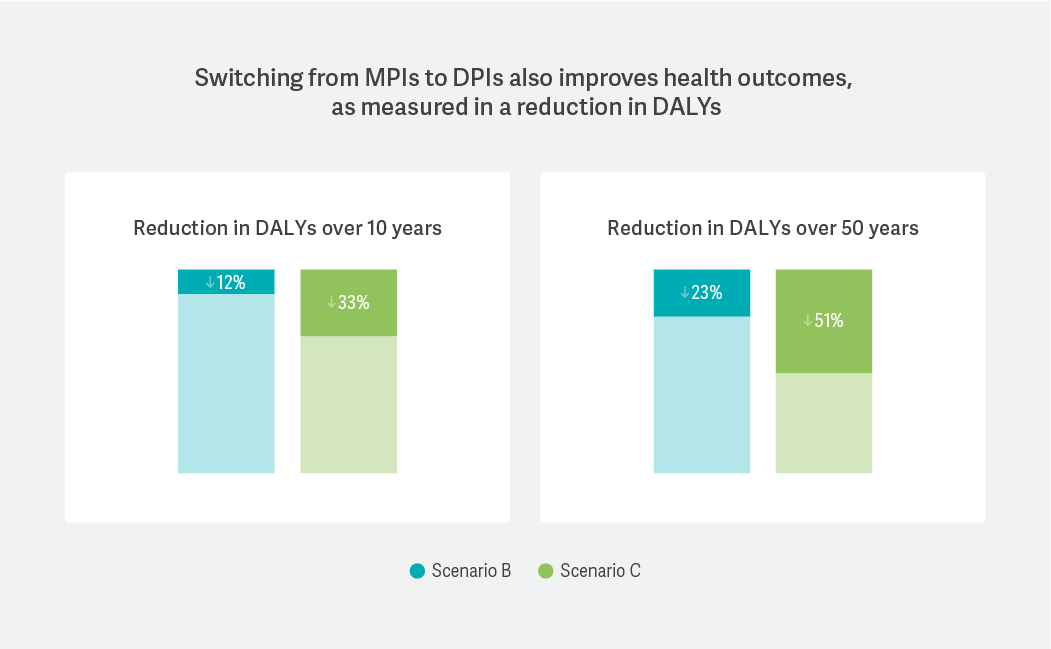
Finally, we estimated the health benefits that flowed from reducing the carbon footprint of inhalers by translating changes in GHG emissions into disability-adjusted life years (DALYs), a commonly used measure of health impacts. A reduction in DALYs means that more people are living longer with less impact from their symptoms.
We found that, regardless of either substitution rate or timeline, DALYs were reduced for the asthma population, ranging from a low of 12% (2% substitution rate over 10 years) to a high of 51% (5% substitution rate over 50 years).
A Way Forward?
Because the asthma population seems destined to grow in the future, efforts to curb the carbon footprint of inhalers will likely become more urgent in the future. The benefits of using MDIs for asthma treatment should be evaluated in view of their global health consequences. This analysis showed that not only would gradual substitution of MDIs by DPIs have positive effects on emissions and health, but that it could be accomplished at a societal cost similar to that of the status quo. ■
*The impact on the global economy, measured in US dollars, of the emissions of one ton of CO2
James Signorovitch, Managing Principal
Todd Schatzki, Principal
Kalé Kponee-Shovein, Manager
From Forum 2022 and featured in Health Care Bulletin: 2022 Selected Highlights.