-
The Growing Economic Burden of Depression in the United States
The economic ripples of major depressive disorder (MDD) are extensive and disproportionate to the amount spent on the disease itself. For every dollar spent treating depression, an additional $4.70 is spent on direct and indirect costs of related illnesses, and another $1.90 is spent on a combination of reduced workplace productivity and the economic costs associated with suicide directly linked to depression.
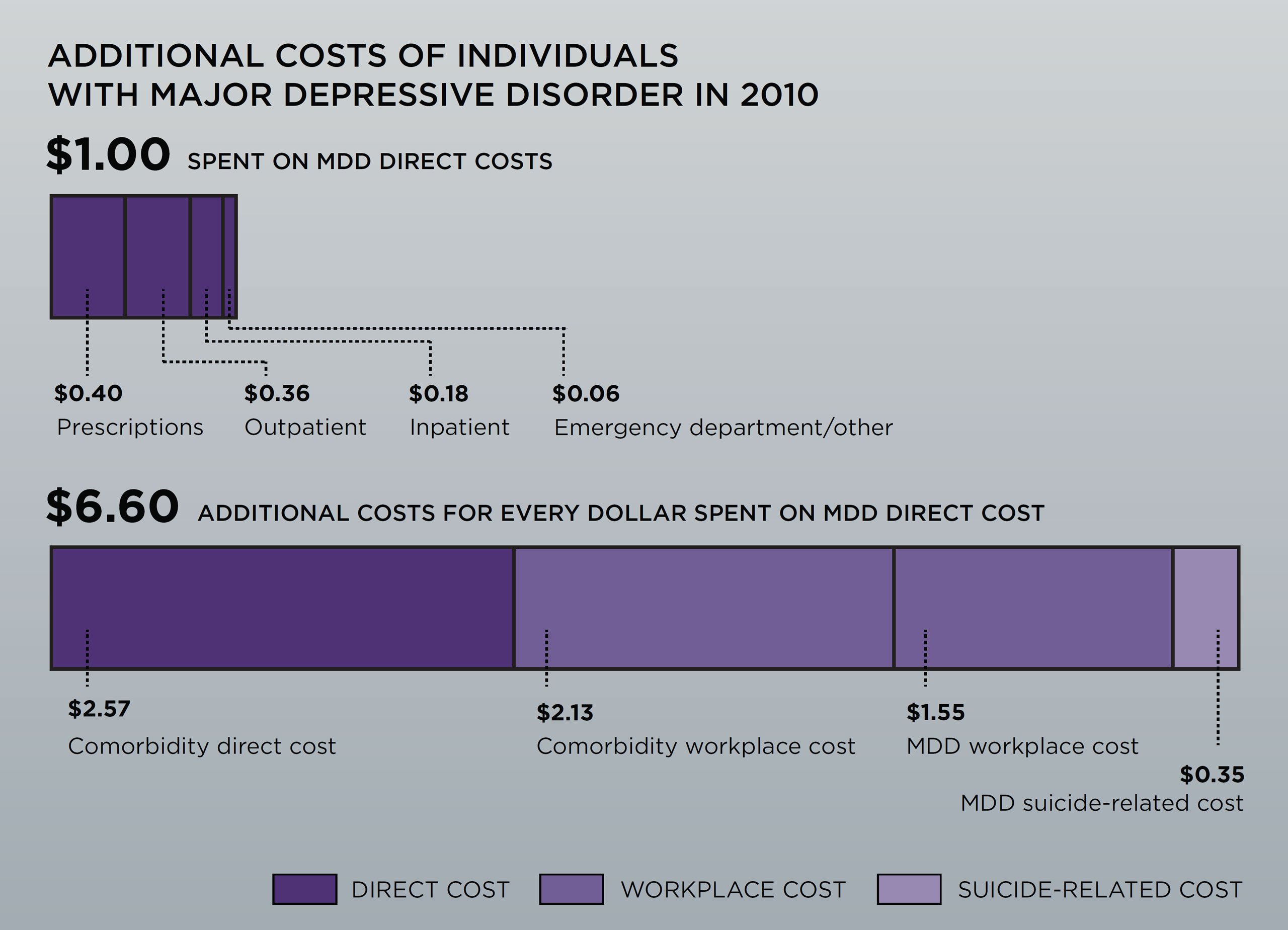
Depression in America now costs society $210 billion per year, according to the newest data available, yet only 40 percent of this sum is associated with depression itself. Looking back after more than 20 years spent studying depression, we now have a much better understanding of the economics of depression in terms of the scale, scope, and mix of attendant costs, as well as the quality of care provided to patients.
Decades ago, when President Clinton introduced his administration’s health care initiative, he tapped Tipper Gore, the wife of the Vice President, to oversee its mental health component. The blockbuster innovation of that era was Prozac, the first selective serotonin reuptake inhibitor (SSRI), which was approved by the Food and Drug Administration (FDA) in 1987. In those days, depression – like most mental illnesses – was deeply stigmatized and vastly undertreated.
Recognizing the challenges, Prozac’s maker, Eli Lilly, funded a cost-of-illness study to promote awareness of the impact of the disease. We completed this work, and when our findings were released, Mrs. Gore was the public spokesperson for the 1993 study. Ten years later, in 2003, Eli Lilly sponsored an updated assessment of the economic burden of depression. In this second study, we found that depression tended to affect people from an early age of onset. Even though many more people with depression were reached in some way by the health care sector, the quality of that treatment was generally not very good. Patients were also being treated far more than ever before by primary care physicians with SSRIs or newer classes of pharmaceutical products.
-
Between 2005 and 2010,
MDD prevalence increased 12% from 13.8M to 15.4M in the adult population
Direct costs increased 27.5% from $77.5B to $98.9B for individuals with MDD
-
In 2015, with our newest study (which received no outside funding), we have documented a rising societal burden of depression, primarily due to a combination of US population growth, an increasing disease prevalence rate, and higher treatment costs per patient. Most of the costs of depression are for related mental illnesses, such as anxiety and post-traumatic stress disorder, as well as for physical illnesses, such as back disorders, sleep disorders, and migraines. We also examined how depressed employees fare at different points in the business cycle. It turns out that during robust macroeconomic times, depressed people tend to be highly employable. But when a cyclical downturn occurs – as was the case during the recent Great Recession – employees with depression tend to be more likely to lose their jobs than their non-depressed counterparts.
With better data on direct and indirect costs, as well as treatment choices and their corresponding consequences from both a health care utilization and an employment perspective, we hope to shed new light on the importance of different levers available to reduce the economic burden of this disease. Such insight will enable the health care system to better direct resources and improve the lives of those living with depression. ■
-
Paul Greenberg is a managing principal in the Boston office and director of Analysis Group’s Health Care practice.