-
A Real-World View of the Health Care Costs of Air Pollution
Our research into the health impacts of air pollution shows that the EPA’s standard cost estimation tool underestimates related health care costs by as much as 40%.
Being able to quantify the link between air pollution and health- and productivity-related costs is important for local, state, and federal organizations seeking funding for pollution-reducing programs, as well as for policymakers and legislators dealing with climate change and other environmental concerns.
To support programs and policymaking, the US Environmental Protection Agency (EPA) developed and maintains an open-source tool called the Benefits Mapping and Analysis Program–Community Edition (BenMAP-CE). According to the EPA, the tool is useful to anyone looking to quantify “the number and economic value of health impacts resulting from changes in air pollution concentrations.”
As the EPA notes in its BenMAP-CE User’s Manual:
“Most users apply the BenMAP-CE tool to answer one of two types of questions:
- What are the human health and economic benefits associated with a policy improving air quality?
- What is the human health burden attributable to total air pollution levels?”
However, in our recent study, we found a large gap between the values produced using the BenMAP-CE methodology and our own estimates of health care costs traceable to conditions exacerbated by pollution levels.
Too narrow a focus
The gap is due to a narrow view of the health impacts of air pollution that underlies the BenMAP-CE tool. The EPA designed the tool to account only for hospitalizations and emergency room visits for certain types of respiratory and cardiovascular conditions, such as asthma attacks and acute myocardial infarctions. The tool also adds on employer costs for work days lost due to the time an employee spends in the hospital or emergency room.
But it is well documented that air pollution’s adverse impacts extend beyond just hospitalization and ER treatment. For example, studies have shown that hospitalization accounts for only a small fraction of the health care costs related to treating asthma patients.1
A 2019 review of the damaging effects of air pollution indicates that the harm to people’s health from air pollution goes beyond the kinds of acute conditions that result in hospitalizations to affect ongoing chronic conditions, “potentially affecting every organ in the body.”2
Our research team, which also included Associate Susan Ou and Senior Analysts Christopher D. Carley and Peter R. Zuckerman, developed a ratio for the increase in total health care costs that were associated with a patient requiring hospitalization for respiratory or cardiovascular conditions, beyond just the hospitalization itself. For example, we found that every patient hospitalized for respiratory care also averaged five additional ambulatory care visits that were not included in the BenMAP-CE tool. These costs account for the impacts of ambulatory care outside of the hospital, such as those shown in the figure.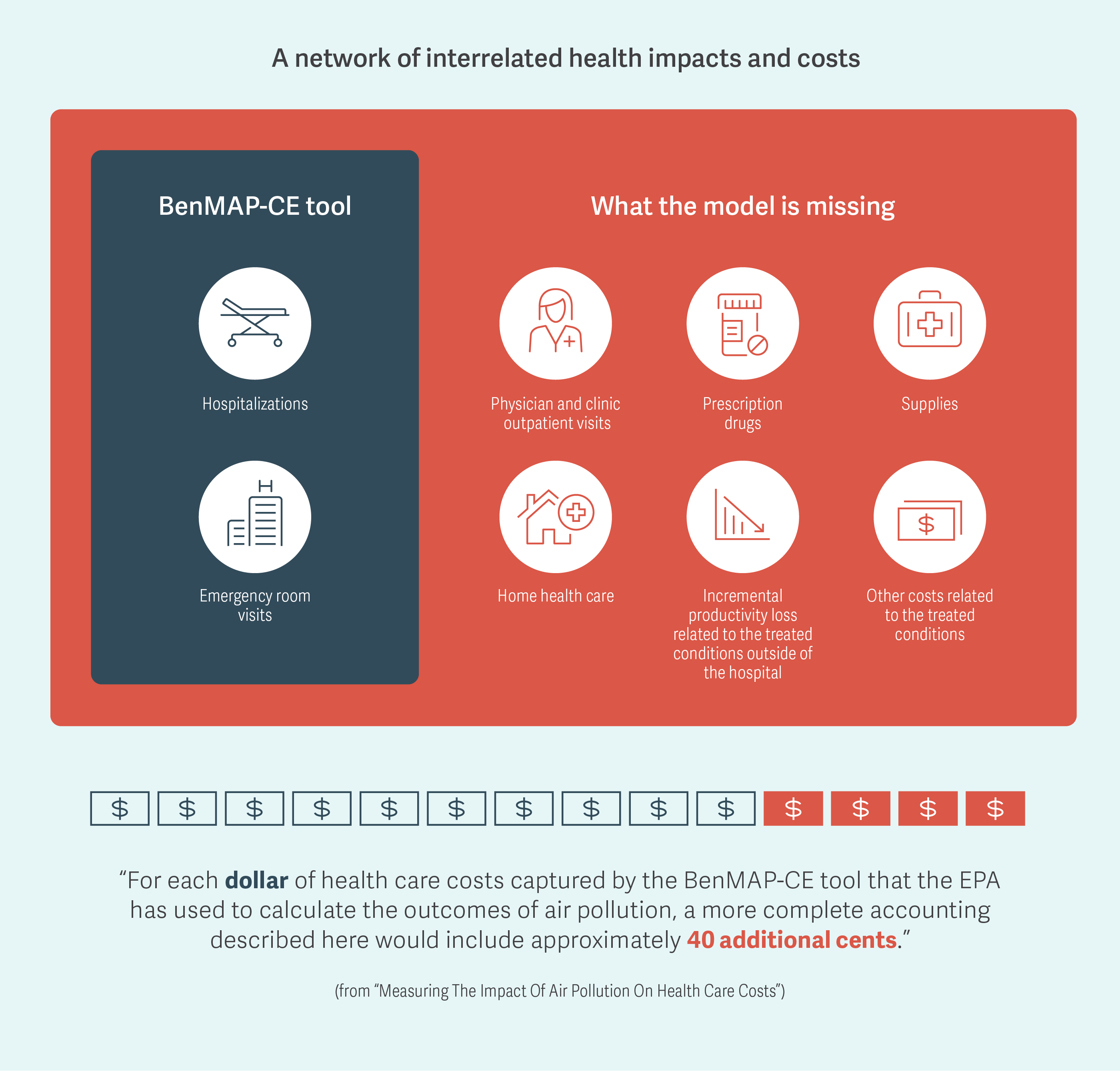
Making a difference for program funding and health care
It is important to quantify accurately the costs of health care associated with air pollution because they add to the financial burden of care paid by patients as well as by private and public insurers. In addition to monetary costs, the need for incremental care in ambulatory and other settings can also add to the already large emotional and time burden on patients dealing with chronic conditions that are further exacerbated by air pollution.
Updating the BenMAP-CE tool to account for the full range of associated care, in addition to hospitalizations and ER visits, would give policymakers, service providers, and payers a more realistic view of the real-life impacts that an increase in air pollution has on patients and employers. In turn, understanding the total impact is vital for improving our ability to estimate the benefits from making concerted efforts to reduce air pollution. ■
-
A note on Analysis Group’s approach
Using OptumHealth’s publicly available claims database of approximately 20 million privately insured people, our team identified a set of patients who had been hospitalized for respiratory or cardiovascular issues in 2016, but had not been hospitalized for the same conditions in 2015. We then calculated the total health care resources used and related costs for these patients in each year. The difference between the annual costs allowed us to develop a ratio for the incremental health care costs associated with a hospitalization.
-
Howard G. Birnbaum, Senior Advisor
Urvi Desai, Vice President
Adapted from Howard G. Birnbaum, Christopher D. Carley, Urvi Desai, Susan Ou, and Peter R. Zuckerman, “Measuring The Impact Of Air Pollution On Heath Care Costs,” Health Affairs, Vol. 39, No. 12, December 2020Endnotes
- Nurmagambetov T, Kuwahara R, Garbe P. “The economic burden of asthma in the United States, 2008–2013.” Ann Am Thorac Soc. 2018; 15(3):348–56.
- Schraufnagel DE, Balmes JR, Cowl CT, De Matteis S, Jung S-H, Mortimer K, et al. “Air pollution and noncommunicable diseases: a review by the Forum of International Respiratory Societies’ Environmental Committee, Part 1: the damaging effects of air pollution.” Chest. 2019; 155(2):409–16.